Understanding the Intricacies of TMS Therapy Billing
Transcranial magnetic stimulation (TMS Therapy) is a more holistic approach now used by many health care providers in the outpatient setting to treat mental health conditions. However, integrating TMS into outpatient healthcare
practices requires a deep understanding of the patient intake and prior authorization process and
medical billing services. This article will explore the complexities of
TMS therapy billing, including coding, documentation, compliance, and new developments in the field.
OVERVIEW OF TMS THERAPY & BILLING PRACTICES

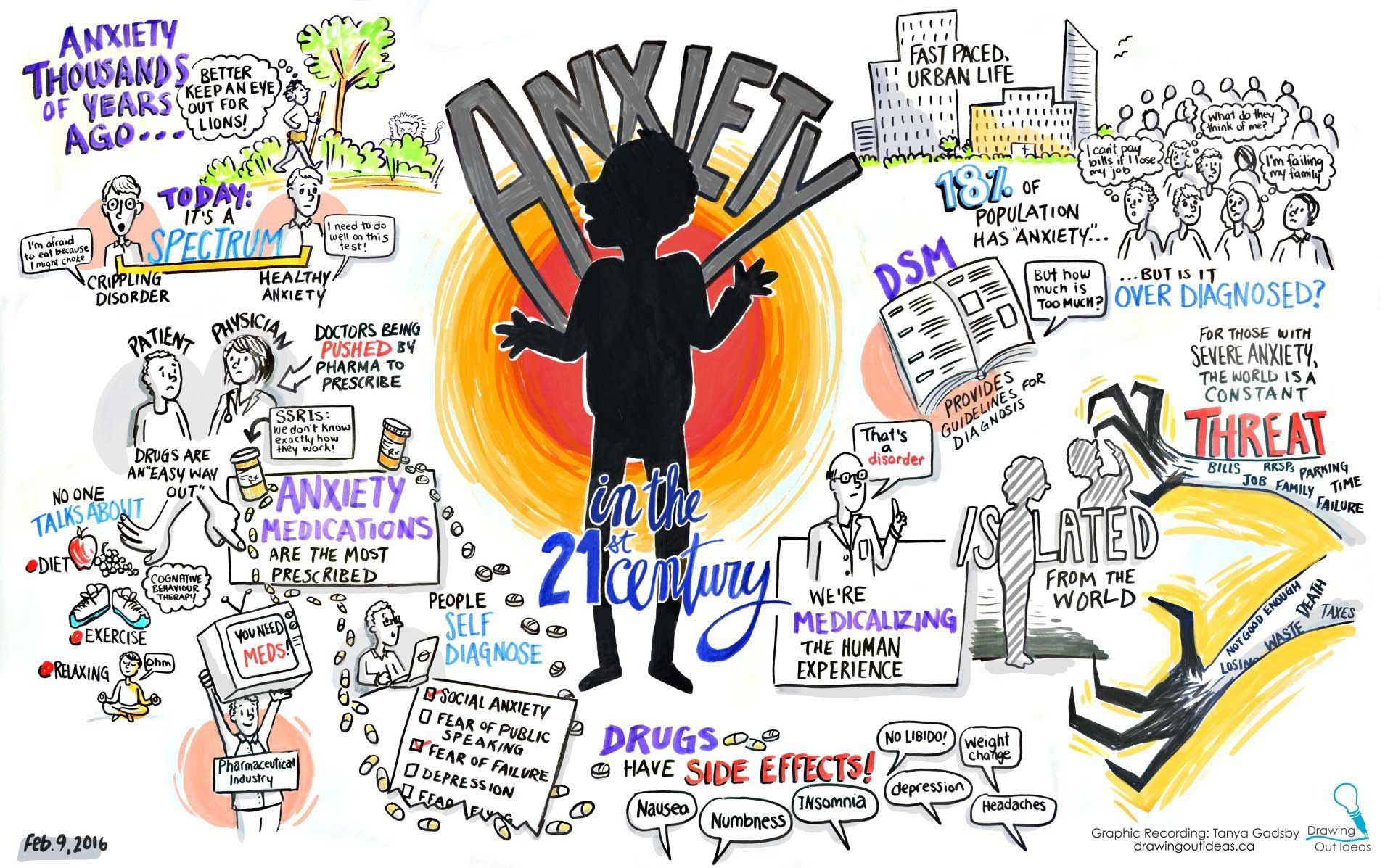
TMS uses electromagnetic pulses to target certain parts of the brain, providing a non-invasive solution for depression and obsessive-compulsive disorder (OCD). TMS is also used to treat other conditions, such as anxiety and various mental health conditions, but is typically not reimbursed by insurance. With the increasing popularity of TMS therapy, healthcare professionals need to handle the intricacies of medical billing to maintain the financial stability of their clinics.
Precision in medical billing is essential for the success of healthcare practices, especially for those offering TMS therapy treatment. Ensuring accurate billing is crucial not only for financial reasons but also to
comply with regulations. Proper billing practices facilitate fair compensation for services rendered while upholding contractual obligations between insurers and providers.
Common Challenges in TMS Therapy Billing
The process of billing for TMS therapy presents distinct challenges that healthcare providers need to address effectively. These challenges range from:
- coding inaccuracies
- insurance denials
- providing treatments outside the prior authorization dates, and
- poor documentation
These challenges require providers to have the skills to recognize and resolve them. Specific challenges include maintaining precise records of treatment sessions and understanding the complexities of insurance regulations pertaining to TMS therapy.
To reduce TMS therapy claims denials, it is vital to implement the following:
- Implementing a comprehensive review process: Establish a thorough review process to ensure that all claims are meticulously examined for accuracy and compliance with policy requirements. This includes verifying patient eligibility, reviewing medical records, and confirming that the treatment provided aligns with the approved treatment guidelines.
- Enhancing communication with healthcare providers: Improve communication channels with healthcare providers to ensure clear and timely exchange of information. This can be achieved by implementing electronic health records (EHR) systems, which facilitate the sharing of patient information across different healthcare settings.
- Implementing a comprehensive quality assurance program to ensure adherence to processes and minimize errors.
- Providing thorough documentation and clear communication with healthcare providers and patients to reduce misunderstandings and disputes.
- Regularly reviewing and updating procedures to align with current best practices and regulations.
- Implementing a patient intake and TMS prior authorization process and onboarding checklist to minimize errors and claims denials
- Defining the roles and responsibilities of the TMS therapy technician. The TMS technician's role is multifaceted, encompassing a wide range of responsibilities crucial to not only a good outcome for the patient, but also to ensure that claims are not denied. These responsibilities include:
- Patient intake process and procedure
- Defining the roles and responsibilities of the TMS technician
- Utilizing TMS treatment room tools for the TMS technician to keep track of prior authorization dates, missed treatment sessions, and monitoring of depression and anxiety screening assessments
Understanding current billing procedures for TMS is vital. Many providers mistakenly believe that billing is simple due to the limited number of CPT codes for TMS treatment. However, the challenge often lies in resolving denied claims that are unrelated to how the claim was billed.
From the initial TMS patient registration and confirmation of insurance coverage to the filing of claims and the process of getting paid, every phase demands careful focus. It's important for medical professionals to focus on thorough record-keeping to back up claims and make the billing process smoother.
For assistance with policies and procedures to streamline the TMS patient intake and prior authorization process, visit Metro NeuroHealth to schedule a complimentary consultation.
Coding and Documentation
Specific Current Procedural Terminology (CPT) codes are associated with TMS Therapy. Let’s explore the CPT codes in detail.
- 90867 Therapeutic repetitive transcranial magnetic stimulation (TMS), initial, including cortical mapping, motor threshold determination, delivery and management
- 90868 Therapeutic transcranial magnetic stimulation (TMS) treatment, subsequent delivery and management, per session
- 90869 Therapeutic repetitive transcranial magnetic stimulation (TMS) treatment, subsequent motor threshold re-determination with delivery and management
Proper coding and documentation not only facilitate billing but also contribute to successful insurance claims, thus reducing the likelihood of denials. One of the biggest mistakes that many TMS therapy practices fail to understand is the need for astute documentation with every treatment.
Daily documentation should include:
- Subjective assessment
- Objective assessment
- Weekly or a minimum of bi-weekly depression screening assessment
Imagine your documentation as a collection of photographs. This collection should depict a patient experiencing moderate to severe depression, whose symptoms progressively diminish over a span of 6 to 9 weeks (the duration of TMS therapy treatment). These images, when requested from insurance companies, should clearly paint a picture of the patients’ progress while undergoing TMS treatment. Essentially, these images (or documents) should represent a patient who is gradually improving with each week of treatment.
Insurance Coverage
Understanding the terrain of insurance coverage for TMS is essential for both healthcare providers and patients. There are differences in coverage that exist across various insurance policies. It’s important to know the payer networks guidelines as they relate to transcranial magnetic stimulation to secure pre-approvals and interact efficiently with insurance companies to guarantee smooth payment.
Remember that TMS CPT codes are more than just billing three (3) CPT codes. There are several considerations and variables that can significantly impact whether a claim gets paid. These might include things such as correct modifiers, prior authorization dates, incorrect benefits and eligibility, payer guidelines, etc.
While most insurance networks medical guidelines for TMS are similar, they often leave out other factors that influence prior authorization approvals. For example, the trial dates of medications or the length of remission for a patient with a history of a substance use disorder. The list can be extensive, but the bottom line is the network typically seems to be more inclined to deny a prior authorization request over approving it. Therefore, it is essential to know your patients, request medical records, be familiar with the network's guidelines for TMS therapy, and back up your request with good records to armor yourself well for a peer-to-peer review or appeal. If the medical guidelines do not back the reason for a denial, then you have plenty of legs to stand on when responding to a denied TMS prior authorization request.
Leave the Headaches of TMS Therapy Billing to the Experts
For some healthcare practices, outsourcing TMS therapy billing services may be a strategic decision.
Practical examples showcase how TMS billing is applied in real-life situations. By examining case studies, providers can understand the obstacles encountered and learn from successful billing approaches, offering valuable insights to fellow professionals in the industry.
The landscape of medical billing is dynamic, and TMS therapy billing is no exception. It's essential for billing service providers to remain abreast of emerging trends, such as changes in reimbursement models, medical policy updates, and the impact of evolving healthcare policies on TMS therapy billing practices.
It is recommended to find a billing provider that focuses on TMS therapy billing and has a thorough understanding of the patient intake and prior authorization process. Metro NeuroHealth is a top choice in outpatient and specialty psychiatry billing, with extensive experience in managing TMS therapy clinics to guarantee the success of your practice.
Schedule a Complimentary Consultation
1-833-TMS-HELP (867-4357)
Info@TMSStartitup.com